Less Radiation to Nearby Organs
After undergoing radiation treatment, some tumors may unfortunately recur in the same spot as before. Retreating these tumors with conventional photon therapy can expose nearby organs to yet additional radiation, causing significant challenges since the human body can only withstand a certain amount of radiation over a lifetime.
In contrast, proton therapy has the advantage of depositing minimal radiation into nearby organs. And, because it is so precise, there is less risk of short- and long-term side effects. There is no “exit dose” into the healthy tissues behind the tumor like there is with traditional radiation. So it is an ideal noninvasive treatment option for retreating tumors that have recurred and provides many patients with a new potential chance for cure.
A Leader in Retreating Recurrent Tumors
More than 40% of the New York Proton Center’s patients come for management of difficult-to-treat recurrent tumors, far exceeding the national average of 11 percent. Our renowned experts in this area have advanced the research and lead multiple national and international guideline papers on reirradiation. They include Dr. Charles B. Simone, one of the world’s foremost experts in treating cancer recurrences.
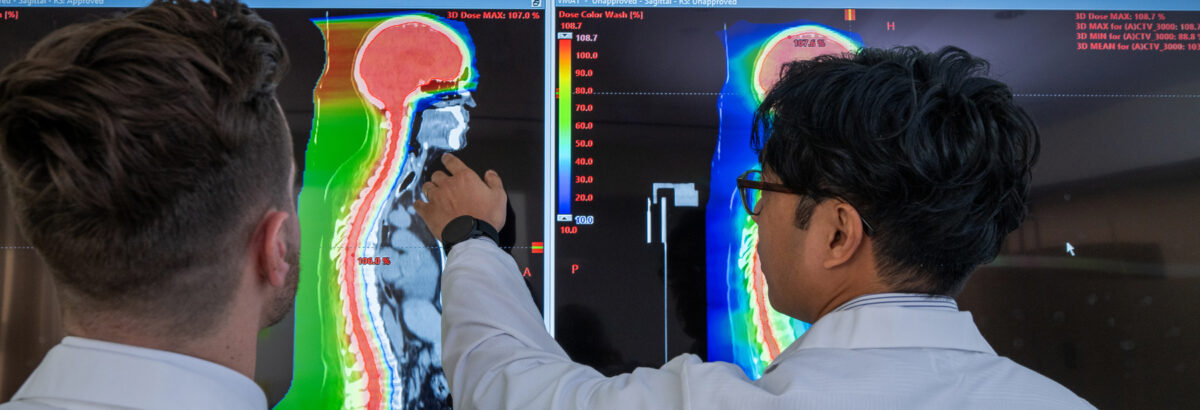
Pencil Beam Scanning at the New York Proton Center
Patients at our center receive pencil beam scanning, a highly sophisticated and the most modern form of proton therapy. It uses an extremely narrow beam of protons to “paint” the intended radiation dose onto the tumor. The technology can target specific parts of the tumor with different radiation dose levels, while better protecting the surrounding normal tissues from irradiation.
Not All Proton Therapy Is Created Equal
Many other proton centers use “volumetric” beams that deliver a fixed quantity of energy to the entire tumor. But the pencil beam scanning technology at the New York Proton Center delivers “intensity-modulated proton therapy,” or IMPT.
Widely considered the most advanced form of proton therapy, IMPT can target different parts of the tumor with different radiation dose levels based on the prescription and the tumor’s exact location, while better protecting the surrounding normal tissues from irradiation. That’s particularly valuable when treating the most complicated tumors, those residing in the fissures of the head, neck and skull base.